Retinal diseases
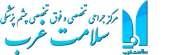
Retinal diseases vary widely, but most of them cause visual symptoms. Retinal diseases can affect any part of your retina, a thin layer of tissue on the inside back wall of your eye. The retina contains millions of light-sensitive cells (rods and cones) and other nerve cells that receive and organize visual information. Your retina sends this information to your brain through your optic nerve, enabling you to see.
Diabetic Retinopathy
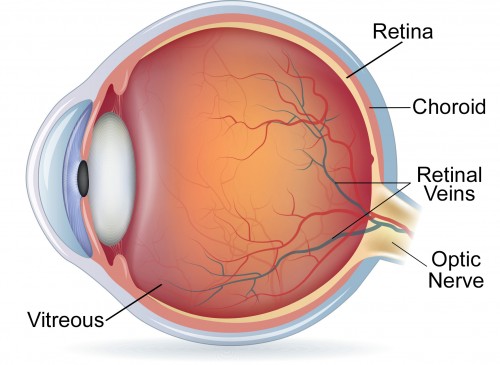
It is an illness that results from diabetes that is because of changes in blood vessel. Diabetic retinopathy is one of complication of diabetes that effects on eyes. Damage of blood vessel in part of sensitivity to sight in eye posterior, means retinal causes diabetic retinopathy. First, it hasn’t any sign or a little eye problems, but at last it makes a person blind.
Different Kinds of Retinopathy
Proliferative Retinopathy
This is a situation when new blood vessel and not natural growth on retinal level. This phenomenon called neovascularization. These new arteries has weaker wall and they are fragile and may leads to blooding. Vitreous is a transparent and like jelly material that fills eye center. Leaked blood makes vitreous teary and relatively sight crossing from pupil to retinal closed. As a result, picture becomes blurred.
This abnormal blood vessel may be changed to a rigid texture that separates retinal from eye posterior and leads to separation of retinal curtain that without curing its decrease sight and blindness.
Abnormal blood vessel can growth around it is (colorful part of eye) and by pressure increase of inside of eyes leads to black water. Proliferative diabetic retinopathy is the most severe illness of retinal arising from diabetes that about 20% people who has diabetes suffering from it.
Symptoms of Retinopathy
Diabetic Retinopathy Complications
Diabetic retinopathy causes growth of abnormal blood vessel in eye retinal. So it leads to serious problem in your sight that is:
1- Eye vitreous blooding
Vitreous is a clear jelly like material that fills middle of eye.
New blood vessel in retinopathy may leads to blooding in vitreous. If blooding is little, there is only stains or black lines in front of eyes (floater). In severe blooding, blood fills vitreous and completely prevents your eyes from seeing. Vitreous blooding doesn’t lead to permanent vision reduction. Sometimes blood cleared in some weeks or some months and your sight becomes like before, unless your eye retinal damaged. At last diabetic retinopathy, glaucoma or both of them leads to complete loss of vision or blindness.
2- Separation of eye retinal
Abnormal blood vessels that grow because of diabetic retinopathy leads to injured texture on retinal. This injured texture stretch retinal from eye posterior and as a result separated it. This complication causes floating stains in eyes (eyes floater), seeing of light spark in eye (eye spark) and severe decrease in sigh too.
3- Glaucoma or black water
New blood vessel that growths in eyes can prevents from natural flow of liquid to out of eyes. As a result, pressure of inside of eye becomes more and leads to glaucoma. This excess pressure leads to damage of optic nerve that brings seen pictures from eyes to brain.
4- Blindness
At last diabetic retinopathy, glaucoma or both of them leads to blindness.
Recognition of Diabetic retinopathy illness
The best way for recognition is eye examination in regular intervals that has been done by ophthalmology. Very severe retinopathy may be without sign. Illness can be cured by treatment. For recognition, optometrist by using ophthalmoscope looks inside your eyes. May be they use eye drop for opening of pupil before examination. If doctor recognizes diabetic retinopathy may be you need colorful picture of end of eye or special experiment by the name of angiography with fluorescein to see that you need treatment or not? In angiography with fluorescein a colorful material injected in your vessel and they took special picture from your eyes.
Diabetic Retinopathy Treatment
If yellow stain damages, may be they use laser for cure. But in ideal situation laser used in first part and for preventing from other damages. For severe part of illness laser or vitrectomy needed. These methods are effective in prevention, fixing or slowdown of sight decrease.
New treatment like injection nonfactor drug us of artery endothelial growth (anti_VEGE) or steroid drugs inside eyes.
Surgery of removing vitreous when there is a blooding inside retina or tear of retina that they are very rare in beginning of this illness. Also vitrectomy has been done in ways that there is scar tissue. Existed treatment for diabetic retinopathy is effective in prevention, delay of sight decrease but they can’t cure illness completely.
People who have treatment should be examined by doctor for any change in eyes regularly. Most of them needs renewal of treatment when illness developments. Also in this illness, Blood sugar control is very important. This subject is true when you are in treatment and your sight becomes better. In reality by useful control of blood sugar one can help for prevention from retinopathy development. Diabetic people if they have any sign of retinopathy should examine by optometrist as soon as possible.
Floater
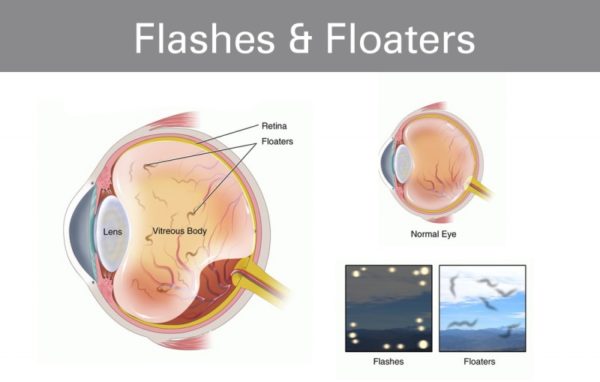
Why floater is created?
Eye sparks
Why is spark generated?
Are floater and spark dangerous?
Are spark and floater curable?
As we said before floater hasn’t a dangerous reason and it doesn’t need to be cure. In most cases after some weeks to months it becomes small and person accustomed to it. But in cases that it is with hole or tear of retinal curtain, person may need cure like laser or surgery for prevention from tear of retinal curtain spark if doesn’t have a dangerous reason, will be fixed after some days or weeks and it doesn’t need to be cured.
Non- ocular reasons of spark
Persons who have migraine experience another type of spark. This spark is zigzag lines that are shaky or big points. Usually these sparks firstly are in center of sight square (it seems in front of a person) and in 15 to 20 minutes, it goes to sideways of sight square, then it disappears. After that headache starts that is one sided and pulsating. But for some people, it has only spark without headache. This condition is eye migraine. One important point is that spark because of migraine is for both eyes but spark of eye problem is only in suffered eye. Another reason of spark is sudden impact crash to head and for this reason, each crash leads that person sees little sparks.
Retina surgery
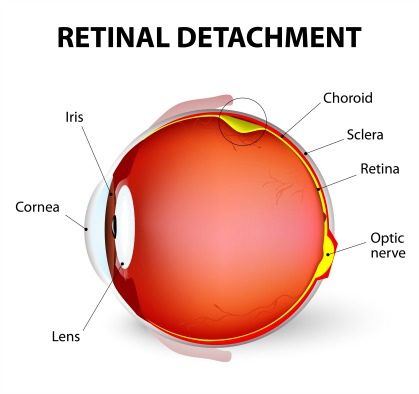
Which person is in danger of retinal detachment?
Symptoms
Survey and recognition of retinal curtain detachment
Treatment of retinal curtain detachment
The only effective treatment is surgery. Retinal detachment does not cure automatically or by drugs and surgery should be done as soon as possible. Kind of surgery is based on place, size, type and kind of retinal detachment, two main things in retinal detachment treatment are:
Closing of holes
Approximating of retinal to down layers and outer wall of eye in a way that retinal can stick on its place.
Based on these, there are different treatment methods for retinal detachment:
Laser Retinopexy
This method is an effective method for closing retinal holes but it couldn’t treat retinal detachment alone. In cases that retinal has hole but retinal isn’t detach, this method can prevent from retinal detachment by closing hole. In this method that is with local anesthesia or with laser (from inside of eye) or by using cryotherapy (from outside of eye) burns created around hole. These burns give adhesion to textures, creates powerful connection between retinal and eye wall. As a result around hole is closed and entrance of liquid to retinal posterior is closed. (Laser creates burning and cryotherapy cold texture and burns it.)
Pneumatic Retinopexy
In this method after local anesthesia, doctor injects a little gas bubbles eyes. This gas bubble dilated inside eyes and push from inside to retinal and put it in its place. Also by putting pressure on edge of retinal holes makes it close and prevent from liquid leakage to retinal posterior. Because gas moving up inside eye, this method is effective when retinal detachment happens in upper part of eye. Because we put gas bubble in right place, we usually recommended patients to put his/her head smooth and sleep in sitting way. Gas bubble usually absorbs in 10 days to two weeks. After this time usually by laser or cryotherapy pen all part of retinal holes burn that hole will not open again.
Scleral buckle
This method is common method in curing retinal curtain detachment. In this method one buckle (a sponger or soft silicon strip by suture sewn to scleral (scroll or eye whiteness) and like a light belt push out wall to inside and make it to go near detachment retinal that retinal can stick in its place. If there is much liquid behind retinal during surgery this liquid discharges that retinal stick fast to outer wall.
In addition during surgery, edge of retinal holes closed by laser or cryotherapy pen. Sclera buckle remains all the time in its place and there is no need to put it out except there is a special problem. Buckle doesn’t see from out and there is no obvious change in eye but because of pressure and change in eye can create myopia.
Viterctomy
In situation that simple methods can’t cure retinal curtain detachment they use a complex surgery by the name of vitrectomy. In situation that holes are very big or very much or a large part of retinal detached, in situation that was blooding inside eyes or retinal is stretched. Usually simple methods are not effective and we should use vitrectomy (it means discharging of vitreous from eyes). In this method first, vitreous with a special instrument discharges from the eye. This special instrument with blade puts vitreous fibers down and discharges them from eyes, and stretch was not on retinal. Also if there is blooding inside eyes, blood washed in this way. Then they inject sterile salt serum inside eyes. At last retinal holes closed by laser. Sometimes for better placing of retinal, heavy liquids (like Perfluoron) injects inside eyes to put retinal in its place. Then this liquid changes with salt serum. Sometimes in addition with salt serum a gas bubble inject in eyes to put upper part of retinal. Sometimes with vitrectomy surgery we use scleral buckle that outer pressure help to closing retinal. In special cases that upper methods are not effective after vitrectomy a special material by the name of silicon oil injects to fill eyeball from inside and put retinal. When it is inside eyes, sight severely disrupted. After some months that retinal sticks with another surgery oil discharges and salt serum injected.
Postoperative care
After surgery especially scleral buckle and vitrectum up to several days, eyes are painful and sensitive. Usually it is needed to use anti-biotic drops up to one to two week and anti-inflammatory drops up to several weeks after surgery. Sometimes other drops (like drugs which decrease eye pressure or drops of pupil). If gas bubble injects inside eyes, person should put his/her head place and for sleeping be in half sitting situation. Altogether after retinal surgery it is necessary that a person regularly goes to doctor for controlling retinal situation and preventing from possible complications.
Surgery result
Surgery result of retinal stick is dependent on two factors:
- Amount of time that retinal was cut from its place.
- Situation of sight center (macula)
Macula or sight center is central part of retinal that is responsible for direct sight. If before surgery, macula wasn’t removed from its place, surgery result is good in a way that more than 2/3 of patients after surgery had enough sight for seeing. But if macula was removed from its place, after surgery patients has weak sight. The best result of surgery is when retinal curtain sticks in its place for one to two weeks. In situations that retinal curtain detachment takes a long time, after surgery the result is not good.
Altogether in 90 to 95% with one or several surgery, retinal sticks in its place, but we should regards that retinal sticks in its anatomy place didn’t improve person sight. As we said sight situation after surgery is dependent on macula and time that retinal was removed from its place.
Generally, whatever retinal curtain detachment were little and was far from retinal Centre, surgery result is better and whatever detachment is bigger and was closer retinal Centre the results is worse.
Prevention from retinal curtain detachment
Rapid recognition is a key of successful cure in retinal detachment. Knowing sight quality in two eyes is very important. It is recommended that all people who are in danger (myopia person, diabetic person, people who has family history of retinal detachment) control their eyes every day.
for doing it they should control each eye sight separately by closing other eye and if there is any change in eye sight they should go to doctor in 24 hours . If you have these signs go to doctor in 24 hours:
Felling of existence of curtain or shadow in front of eyes
Seeing light sparks.
Existence of floater and increase of floater
Seeing grid like things in front of eyes.
Each decrease in sight that is sudden.
Rapid recognition of retinal curtain detachment is the most important factor of successful cure.
Postoperative retinal surgery (retina) care
Retinal surgery is done due to the detachment of the sensory-neural layer of the eye from its underlay and attaching these two layers together.
- Eye Protection
After surgery,use a protective plastic shield for 2 to 3 weeks to protect the eye and prevent any impact to the eye. You can use glasses during the day and shields at night. The plastic shield is washable. Wash it daily and put on your eyes after drying.
How to use and place the shield and how to rest after retinal surgery are very important in the success of the retinal surgery.
The resting position varies different depending on the location of the tear and type of retinal surgery, which is explained to you by the surgeon and must be carefully observed. Sometimes, the prone position resting is recommended depending on the type of surgery. In this case, the patient should sleep on his abdomen while resting. In this position, the forehead and face are looking down.A few days after retinal surgery, the eyelids are usually swollen naturally. Sometimes, especially in the morning, sticky discharge or pinkish serous fluid withdrawal are seen in these patients.To remove the eye dried secretions, first use a few physiologic drops or a drop of chloramphenicol on the eyelids. Then, after softening the secretions,gently and without putting any pressure on the eye itself, cleanse the secretions with cotton or a sterilized gauze.
- Postoperative anti-inflammatory drugs or corticosteroids
The sedatives and anti-inflammatory pills are sometimes used according to the surgeon’s diagnosis, which are often discontinued after one week to ten days after the surgery. The corticosteroids are used to reduce the inflammation and increase the patient’s healing course. Be sure to take your doctor’s advice on how to use them.
- Travel after surgery
Traveling with cars and trains is allowed. For traveling by plane, you should consult with your surgeon if the eye contains gauze.
- Praying
From the day of operation, praying with tayammum is only allowed on the stone.
- Study, watching television and usual activities
Study, watching television and usual activities of life not associated with intense physical activity are allowed.
- Bathing
With attention to the correct way of placing the head, you can wash all of your body except your head and face.If the retinal surgery is not accompanied by a complication, you can get a bath a week after the surgery; but when washing your face and face, you should keep the eyes closed and do not make any pressure on the eyelids. Also,you must use baby shampoo and soap.
- Diet
This disease and its operation do not need a particular diet nutritionally. If the patient had a special diet before the operation (diabetes, hypertension, stomach ulcers, etc.), he should continue the same diet after the surgery.
- Makeup material
Strongly avoid the use of cosmetics (mascara, synthetic eyelashes, colored lenses, oily materials, etc. around the eyes) and ask your doctor when you can begin again to use them. After surgery, retinal re-detachment is possible. In the event of reduced visibility, the elongation of the objectsimage or the blurring of an area from the field of vision or seeing a spark in the eye, immediately refer to your surgeon in the emergency department. The best vision will usually be achieved about 3-4 months after the surgery provided that the retina has been attached and the resulted refractive error has been corrected. Visit your doctor on appointed dates.
- Eye drops
Using eye drops may be needed 1 to 2 months after the surgery. Strongly avoid taking or stopping drugs arbitrarily.Try to use the drops at the time prescribed by your doctor.At intervals of sleep (5-6 hours), you do not need to wake up for using the drops; however, you should ask this from your doctor as well. Read the instruction on how to keep the eye dropson the drug brochure. However, normally, the opened eye drop should be kept at normal temperature (25-30 °C) and use it up to 3 weeks after opening its cap. Thus, avoid the droplets from freezing or extreme heat.
- Correct use of eye drops
First, wash your hands thoroughly with soap and water.Bend your head slightly back, pull your lower eyelid down with your pointer finger to create a small hole.Drop a droplet in the created hole.After dropping the drop, keep your eyes gently closed for two to three minutes.This will help to better absorb of the medicine and reduce its effects.If you need to use two different drops at a time, make an interval of at least five to ten minutes between them. If you notice symptoms such as redness, tenderness, pain, purulent sections and intense eye irritation, see your doctor.